Stroke Recovery Program
The Stanford Stroke Recovery Program is dedicated to improving the function and quality of life of stroke survivors. Based at Stanford University, the Program is uniquely positioned to bridge the barriers between neuroscience, engineering, and clinical research, to develop new therapies for stroke survivors. With grant funding from the Stanford Neurosciences Institute, the Program has brought together world-renowned scientists from a wide variety of disciplines, including stroke neurology, neurosurgery, neuroscience, mechanical, electrical, and bio-engineering, systems and molecular neuroscience, imaging/radiology, neuroimmunology, and genetics.
Our multi-disciplinary team of scientists is constantly innovating to develop new treatments that will improve gait, arm function and cognition after stroke. The medical innovations developed in our laboratories span a wide array, including immune-modulating therapies, stem-cell therapies, non-invasive brain stimulation (TMS), and medical devices developed by Stanford engineers. Being located in the center of Silicon Valley, the worlds most well-known hub for technological innovation, the Program has also established ties with multiple start-up companies that have developed innovative technologies to help patients recover from stroke. Our highly-experienced group of clinical scientists conducts trials to tests how effective these new treatments are at improving the symptoms of stroke survivors.
In addition to advancing research in the field of stroke recovery, we have a strong clinical neurologic rehabilitation program that serves stroke patients from the San Francisco Bay Area and beyond. A multi-disciplinary team of physiatrists, stroke neurologists, stroke nurses, physical therapists, occupational therapists, speech therapists, neuropsychologists, and social workers works together to provide the best care possible for our patients. The outpatient neurological rehabilitation program is based at Stanford Healthcare's state-of-the-art Neuroscience Health Center. The center, designed with the patient in mind, has an expansive gym with specialty equipment for patients with neurological impairments, spacious exam rooms, and convenient parking in the adjacent parking structure. The center is also home to the Neuroscience Supportive Care Program, which provides a variety of free support groups, classes, workshops, personal one-on-one consultations and services that are open to all patients and families in the community regardless of where they receive their stroke care.
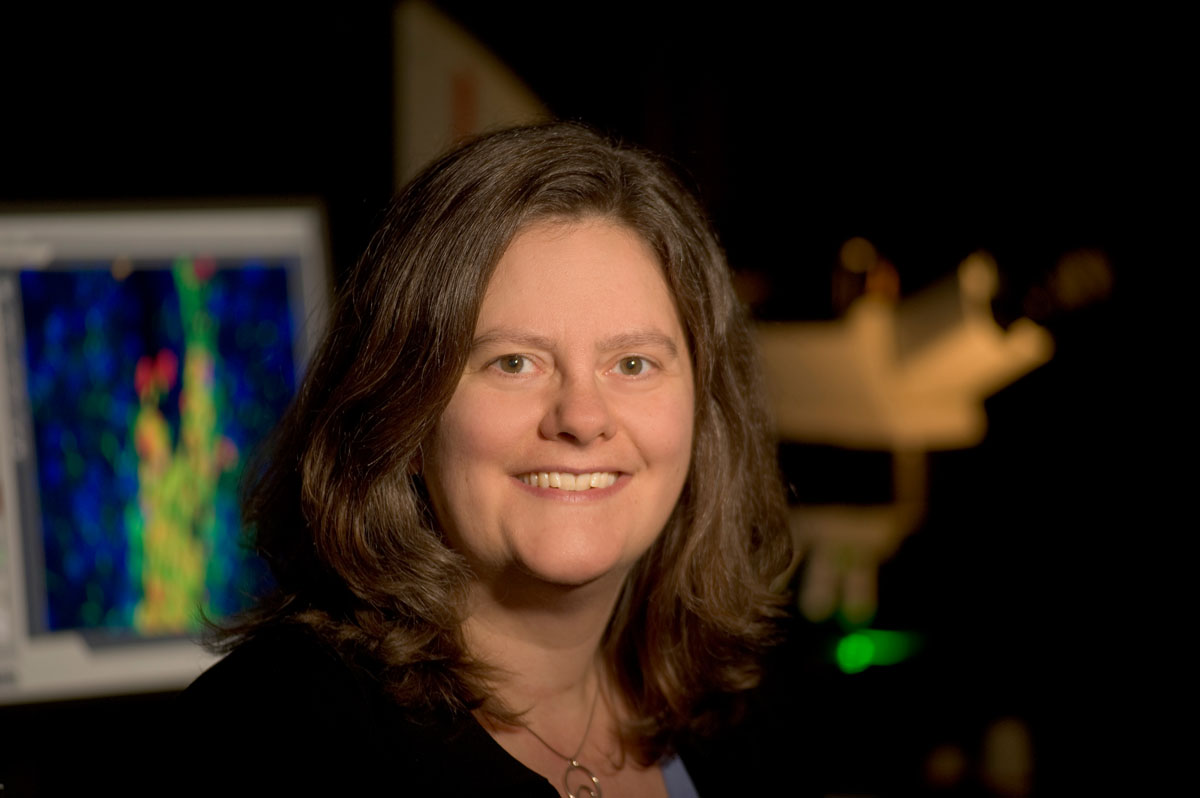
Marion S. Buckwalter, MD, PhD
Professor of Neurology and Neurosurgery
Maarten Lansberg, MD, PhD
Professor of Neurology
Stroke Patient Care
Stanford Health Care’s nationally-recognized Comprehensive Stroke Program provides comprehensive care and treatment for stroke.
When making a donation online please specify the donation is for "Stanford Stroke Recovery Program/Drs Buckwalter and Lansberg"
Contact Us
To inquire about participating in one of our current or future stroke recovery trials, please contact us at: 650-723-8886 or strokerecovery@stanford.edu