Lung cancer is the deadliest cancer an individual can develop. Worldwide, and in the US, it remains the leading cause of cancer-related deaths by far, with most patients diagnosed at an advanced stage when curative treatments are lacking. In the past, the largest role radiation therapy has played in lung cancer treatment has been for palliative care in these late stages. However, within the past couple of decades, the field of oncology has witnessed a shift to more curative treatments for patients with lung cancer, with radiation being a key factor in this new trajectory.
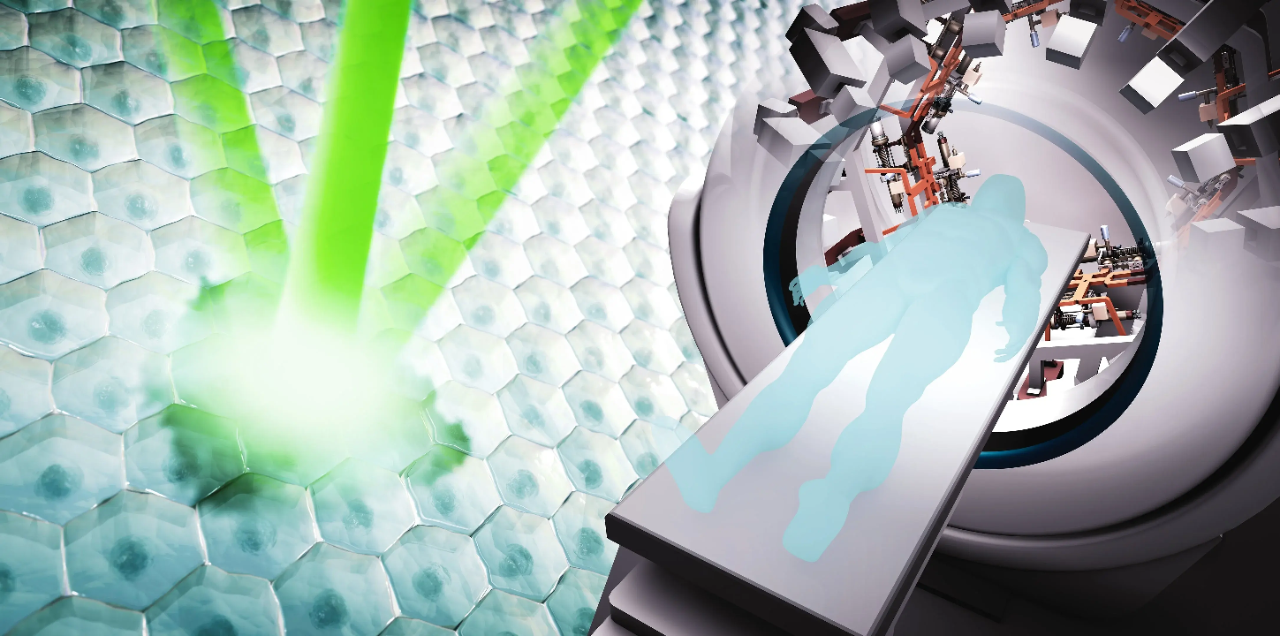
PHASER (pluridirectional high-energy agile scanning electron radiotherapy) is a novel approach for radiotherapy treatment of cancer patients. What sets PHASER apart from similar radiotherapy machines in the field is its approach to motion management. While promising modalities like biology-guided radiotherapy and MR-guided radiotherapy techniques maintain increased visualization of the tumor, PHASER aims for speed, in the form of “flash” treatments: zapping tumors with high-energy X-rays. A major problem when treating tumors in the thoracic region is bodily movement. This is especially true in lung tumors, which can make precise irradiation of lung tumors a difficult task due to natural movement as a patient breathes. Utilizing PHASER technology has the potential to cut out the risk of irradiating surrounding healthy tissue by delivering treatment in less than one second- leaving no time for any significant or disruptive motion. Currently, the only feasible form of flash treatment in the field is for skin cancer tumors.
Looking ahead, reaching deeper organs with a highly focused dose becomes possible with PHASER technology.
“Even though there is less damage to normal organs, there is not less damage to tumors, so it’s at least as good,” said SCI Member Bill Loo, MD, PhD, professor of radiation oncology. “That is the holy grail of cancer therapy.”
In addition to faster radiotherapy treatment, there is further hope that delivering one concentrated dose of radiation will have a greater effect on the tumor itself, compared to delivering the same dose amount with the current standard of technology.
This technology is made possible by our collaboration with the Accelerator Research Division at Stanford Linear Accelerator Center (SLAC) National Accelerator Laboratory. We realize that by developing this technology, we also have a responsibility to share it with the world. In fact, around 50% of cancer patients worldwide who would benefit from radiotherapy do not have ready access to treatment. SLAC has pioneered an entirely new class of accelerator, promising a drastic cut in manufacturing costs while boasting heightened power efficiency and stronger beam capabilities.
Furthermore, PHASER machines will be designed to be compatible with existing infrastructure found in a standard clinical setting. Our goal is to make this curative cancer care globally accessible.
Radioactive advances in lung cancer treatments
“The majority of patients with lung cancer have historically been considered incurable, but more and more, we’re actually seeing these patients cured. That’s led to a really big shift in thinking about lung cancer,” said Loo.
Even combined with an aggressive combination of chemotherapy, historical cure rates were below 10% for patients with regional disease. However, with recent advances in the field, Loo sees opportunities for cure where they did not exist previously.
“We’ve seen tremendous advances in the ability to effectively treat locally advanced lung cancer. In combination with chemotherapy and immunotherapy, we’ve seen the cure rates increase to nearly the 40-50% range, which was unimaginable in years past. There’s still a lot of room for improvement, but it’s a completely new ballgame,” he remarked.
With regard to the contribution of radiotherapy, he attributes the improved odds to two clinical facets: improved imaging and improved radiation delivery.
With the ability to obtain better visualization of the target, physicians are able to deliver a more precise and potent dose of radiation, minimizing the dose to the surrounding healthy tissue while concentrating on the tumor.
An even newer paradigm shift expanding effective treatment to other stages of lung cancer, from early to advanced, is a direct result of a novel treatment technique known as stereotactic radiotherapy. Stereotactic ablative radiotherapy (SABR) is highly focused radiation treatment that gives an intense dose of radiation concentrated on a tumor, while limiting the dose to the surrounding organs. Since its development and refinement, it has become a treatment of choice for many people with limited volume tumors for whom surgery may not be an optimal treatment.
In early stages, surgery is a very effective treatment for lung cancer, with an average cure rate of around 70%. However, even if lung cancer is caught early, surgery isn’t an option for many patients who have other underlying health complications, like cardiovascular disease or emphysema. That’s where SABR comes in: “With this highly focused image-guided radiotherapy, we are now able to give a really high “ablative” dose of radiation safely to these smaller tumors,” Loo asserted. In the past, with less focused radiation, much of the surrounding healthy tissue would receive the same dose as the tumor, preventing the use of ablative doses that would cause excessive damage. Now, with the advent of SABR, our team can safely administer highly ablative doses of radiation to inoperable patients, giving them a non-invasive and comfortable option where there wasn’t one before. Furthermore, SABR and other focused radiation techniques can now be used even to treat patients with a limited extent of late stage lung cancer that has metastasized to other body regions.
“Cure is no longer off the table for many of these patients. That’s a really big shift in thinking about lung cancer” Loo said.
April 2024
By Kai Zheng