February 10, 2006
STANFORD, Calif. — Norman E. Shumway, MD, PhD, the father of heart transplantation and one of the pre-eminent heart surgeons of his time, died Feb. 10 at his Palo Alto home of complications from cancer, the Stanford University School of Medicine announced. He celebrated his 83rd birthday the previous day on Feb. 9.
Shumway, professor emeritus of cardiothoracic surgery, performed the first successful human heart transplant in the United States in 1968 at Stanford. The recipient, 54-year-old steel worker Mike Kasperak, lived for 14 days.
The landmark operation created a burst of enthusiasm for heart transplantation, though cardiac surgeons quickly lost interest because of the high rate of post-surgical deaths.
Shumway nonetheless persevered in the field amid controversy over legal and economic issues, particularly the issue of what constitutes brain death among potential donors. For nearly a decade, Stanford stood virtually alone as the only center performing the pioneering operation. Shumway and his colleagues made steady progress, paving the way for a procedure considered routine today.
“Many people gave it up when they thought it was too difficult, but Dr. Shumway had the persistence and vision that it could work. His determination to make heart transplantation work was absolutely crucial,” said Bruce Reitz, MD, the Norman E. Shumway Professor of Cardiothoracic Surgery at Stanford and former chair of the department.
Nearly 60,000 patients in the United States have enjoyed longer lives because they received new hearts through transplant programs at some 150 medical centers around the country. At Stanford, some 1,240 patients have benefited from heart transplants.
Shumway, a reticent man who did not like to tout his accomplishments, told a crowd of transplant patients at a 2003 Stanford reunion that it was “gratifying to see the changes that have made this (heart transplant) an almost ordinary experience.” At the reunion party, which also marked his 80th birthday, he praised the patients, saying, “You made us look good.” He called them “the real heroes … so marvelous, so strong, so courageous.”
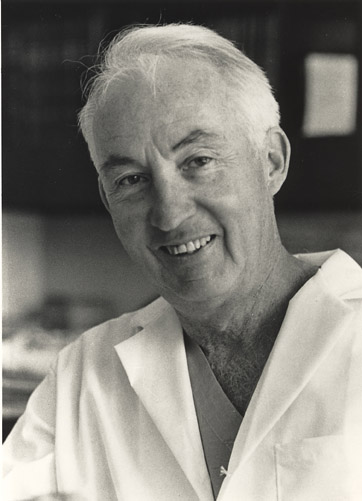
Norman Shumway, MD, PhD, was the father of heart transplantation and one of the pre-eminent heart surgeons of his time.
Philip Pizzo, MD, dean of Stanford School of Medicine, called Shumway “one of the 20th century’s true pioneers in cardiac surgery.”
“He developed one of the world’s most distinguished departments of cardiothoracic surgery at Stanford, trained leaders who now guide this field throughout the world and created a record of accomplishment that few will ever rival. His impact will be long-lived and his name long-remembered,” Pizzo said. “We will miss Norm Shumway and the dignity and excellence that he brought to medicine and surgery — and to Stanford.”
Shumway, the Frances and Charles Field Professor of Cardiovascular Surgery, Emeritus, cherished the fact that he had trained so many of the world’s leading cardiac surgeons who went on to direct departments of their own at major medical centers. His approach, contrary to the conventions of the time, was to step back from the spotlight and give his young trainees major responsibility in the operating room, greatly improving the learning experience.
“I never worked so hard in my life and never learned so much and had so much responsibility at a young age,” said William Brody, MD, PhD, president of Johns Hopkins University and a Shumway trainee. “He was a brilliant teacher and a master psychologist. With his humor, he always made it fun. To be in the operating room with Shumway was the height of your day because he was brilliant and witty. At a time when everybody made cardiac surgery seem complex, he made it seem easy.”
Shumway, who was born in Kalamazoo, Mich., did not start out to become a physician. He entered the University of Michigan in 1941 intending to study law but left two years later after being drafted into the Army. In the military he was given an aptitude test that asked him to check a box for a career interest: medicine or dentistry. He chose the first and was enrolled in a specialized Army program that included pre-medical training at Baylor University in Texas. He moved on to Vanderbilt University, where he received his MD in 1949.
He did his internship and residency at the University of Minnesota, where he developed an intense interest in cardiac surgery. After another two-year stint in the military, this time the Air Force, he continued his surgical training in Minnesota and obtained his PhD in cardiovascular surgery in 1956.

Shumway (left) and Donald Harrison meet the press after they perform the first adult human transplant in the United States on Jan. 6, 1968. The recipient, 54-year-old steel worker Mike Kasperak, lived for 14 days.
Shumway came to Stanford in 1958 as an instructor in surgery. Shortly after his arrival, the medical school moved from San Francisco to Palo Alto, giving Shumway the opportunity to launch the cardiovascular surgery program at the new, expanded campus.
In 1959, working with then-surgery resident Richard Lower, MD, he transplanted the heart of a dog into a 2-year-old mongrel. The transplanted dog lived eight days, proving it was technically possible to maintain blood circulation in a transplant recipient and keep the donated organ alive. Shumway and his colleagues would spend the next eight years perfecting the technique in dogs, achieving a survival rate of 60 to 70 percent.
“We started out doing this as a technical exercise and the animals began to survive,” he said years later.
In 1967, he announced that he was confident enough in the research to start a clinical trial and that Stanford would perform a transplant in a human patient if a suitable donor and recipient became available. Shortly thereafter, Christiaan Barnard, MD, of South Africa performed the world’s first heart transplant on a patient who lived for 18 days, using the techniques Shumway and Lower had developed.
On Jan. 6, 1968, Shumway did his landmark first procedure which — to his chagrin — attracted worldwide media attention, with journalists climbing the walls of the hospital to try to get a peek into the operating room.
Years later, Shumway said of the transplant: “We put in the heart and nothing happened. There were slow waves on the EKG and then the heart began beating stronger and then exuberance…. We knew we would be okay.”
Edward Stinson, MD, the then-chief resident in cardiac surgery who assisted Shumway, described the operation as “pretty awe-inspiring.”
“After we removed the recipient’s heart, we stared at the empty pericardial cavity and wondered what we’d actually done,” recalled Stinson, professor emeritus of cardiothoracic surgery at Stanford. “His (Shumway’s) wit always came through, no matter how challenging the circumstances. He said, ‘I’m not sure. Time will tell.’ We proceeded with implanting the new heart. It was pretty exciting to see it start up.”

At the 2004 transplant reunion, Shumway (right) talks with Danilo Oncena, who underwent two heart transplants at Stanford. It was the last such reunion that Shumway attended.
Shumway and his colleagues made steady progress over the next decade through careful selection of donors and recipients, efforts to increase the donor pool, improvements in organ preservation and in heart biopsies and advances in drugs to prevent rejection of the foreign organ, among other developments. His team was the first to introduce cyclosporine for heart transplantation in late 1980. With the availability of immunosuppressive drug, which is still in use today, the field took a giant leap forward.
In 1981, Shumway and Reitz performed the world’s first successful combined heart-lung transplant in 45-year-old advertising executive Mary Gohlke, who lived five more years and wrote a book about her experiences. By the late 1980s, they were transplanting hearts into infants as well.
Shumway rose to become chief of the division of cardiothoracic surgery at Stanford in 1965 and in 1974, he negotiated the creation of a separate Department of Cardiothoracic Surgery, which he chaired until his retirement in 1993.
His accomplishments were not limited to the field of transplantation. Shumway also made significant contributions to treatment of congenital heart problems in children, as well as valve problems and aneurysms in adults.
Over the years, Shumway received dozens of honors and awards. In 1980, he was named honorary president for life by the International Society of Heart and Lung Transplantation. He also has received the Scientific Achievement Award from the American Association for Thoracic Surgery, the American Surgical Association, and the American Medical Association, as well as the Trustees Medal for Distinguished Achievement from Massachusetts General Hospital, to name a few.
He is survived by his former wife, Mary Lou, of Palo Alto; four children—Sara, Lisa, Amy and Michael; and two grandchildren. The family requests that any memorial donations be made to the Stanford University Heart Transplant Patient Care Fund, in care of the Department of Cardiothoracic Surgery, 300 Pasteur Drive, Falk Building, Stanford, CA, 94304-5407.
About Stanford Medicine
Stanford Medicine is an integrated academic health system comprising the Stanford School of Medicine and adult and pediatric health care delivery systems. Together, they harness the full potential of biomedicine through collaborative research, education and clinical care for patients. For more information, please visit med.stanford.edu.