Welcome to the Division of Sleep Medicine
Outstanding patient care, innovative sleep medicine research, educational excellence, and commitment to our community
Our division encompasses the best that the fields of sleep, sleep medicine, and translational sleep science have to offer. Our clinical faculty and staff have the privilege of diagnosing and managing patients with a diverse range of sleep disorders using a personalized and patient-centered approach. Additionally, our researchers are exploring new frontiers of sleep and circadian science, exploring investigative areas of basic science to complex sleep disorders. Starting with the world’s first sleep clinic and laboratory here at Stanford in 1972, we have emerged as the foremost international center for the study of sleep and the management of sleep disorders. We hope that you will join us in our journey to develop new sleep disorder diagnostic tools and treatments, to continue to drive our specialty forward, and to answer fundamental questions about sleep, including the question that comprises the holy grail of our field… “why do we sleep?”
History
The Division of Sleep Medicine at Stanford University has garnered global recognition for sleep-related advancements in patient care, research, and education, and is a recognized leader in the management of sleep disorders. The Division has a storied history that had its origin in 1972 as the world’s first sleep clinic and laboratory; since then, Stanford Sleep Medicine is recognized as one of the world’s largest and best-known sleep centers. The Stanford Sleep Medicine Center is housed in our state-of-the-art facility, which contains advanced equipment for the diagnosis and treatment of the 90 different sleep disorders, and includes 14 clinic bedrooms and 4 research bedrooms for overnight in-laboratory sleep studies.
We provide outstanding, personalized care using the most advanced and effective techniques in managing sleep disorders from infancy through old age, such as cognitive behavioral therapy for insomnia and the latest devices and surgical treatments for obstructive sleep apnea. We also offer specialized clinics for narcolepsy and hypersomnias; neuromuscular disease; obesity-hypoventilation; sleep apnea bariatrics, dentistry, and surgery; restless legs syndrome and other movement disorders; sleep and chronic obstructive pulmonary disease; sleep and memory issues; sleep and autonomic dysfunction; and insomnia.
Our goals are to continue building a structure of personalized care and integrated medical approaches, with the overall intent to improve the lives of patients with sleep disorders. We will continue to deliver optimal care for our patients, develop new sleep-related technology, encourage clinical and research collaboration in other areas of medicine, share and disseminate our knowledge to our patients and other stakeholders, and train future leaders of our field.
In the Media
- 12/04/2020 – STAT
How climate change could chip away at sleep health
Some experts predict that heat-related disruptions to sleep will likely get worse in the years to come as nighttime temperatures rise. Rafael Pelayo, clinical professor of psychiatry and behavioral sciences, discusses how climate change can affect the way people sleep.
- 12/01/2020 – Stanford News
SLAC, Stanford scientists recognized for breakthroughs at Falling Walls competition
Seven SLAC and Stanford nominees were finalists in the 2020 Falling Walls Breakthroughs of the Year competition. The annual event brings together researchers, scientists, engineers, innovators and thinkers from around the globe to discuss science, politics, business and media. Sergiu Pasca, associate professor of psychiatry and behavioral sciences, was a top 10 category finalist on the topic of “Human Neuropsychiatric Disorders.”
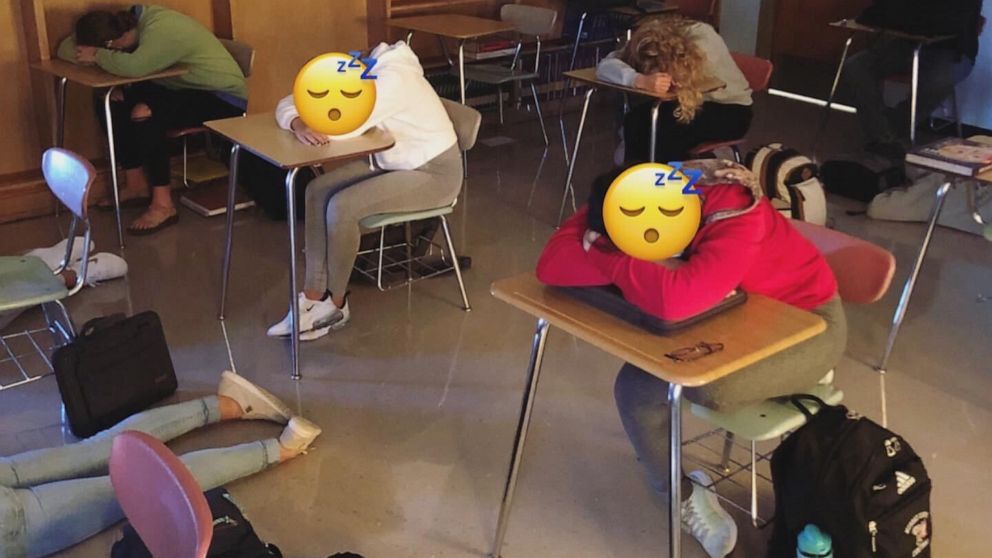
- 10/21/2020 – Good Morning America
Why this high school teacher lets his students sleep in class
This story discusses a Minnesota teacher who allows students to sleep during class, as part of a unique sleep study lesson. Rafael Pelayo, clinical professor of psychiatry and behavioral sciences, provides comment here.
- 10/12/2020 – Spectrum | Autism Research News
Brain organoids reveal neuronal flaws in syndrome tied to autism
Neurons derived from people with 22q11.2 deletion syndrome show deficits in calcium signaling and electrical activity, pointing to possible therapeutic targets. New findings uncover factors that may contribute to the development of psychiatric conditions associated with 22q11.2 deletion syndrome. They could also help researchers identify new therapeutic targets - Sergiu Pasca, associate professor of psychiatry and behavioral sciences, is quoted in this article.
- 09/28/2020 – News Center
Stanford scientists solve secret of nerve cells marking a form of schizophrenia
A common genetic deletion boosts the risk for schizophrenia by 30-fold. Generating nerve cells from people with the deletion has showed Stanford researchers why. Sergiu Pasca, the Bonnie Uytengsu and Family Director of the Stanford Brain Organogenesis Program and an associate professor of psychiatry and behavioral sciences, is senior author.