Bio
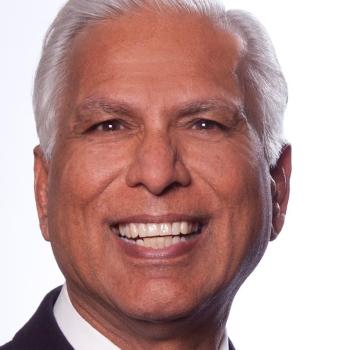
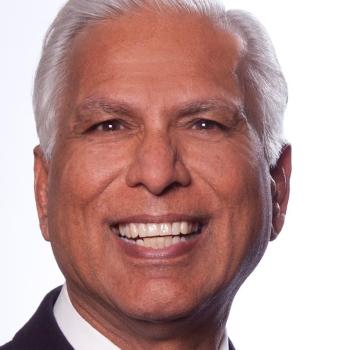
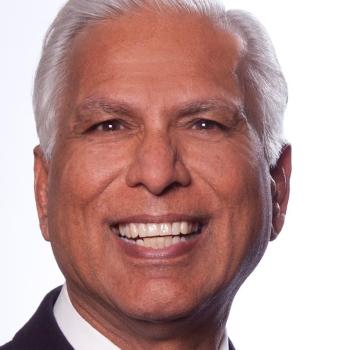
Vinod K. Bhutani, M.D. FAAP a graduate from Armed Forces Medical College, India is currently the Professor of Pediatrics (Neonatology, Emeritus) at the Stanford University School of Medicine. He is a board-certified Neonatologist and formally trained as a pulmonary physiologist, transformational bilirubin biologist and pediatric health policy expert. His primary career aims encompass distinct investigative domains: i) clinical translation of basic science; (ii) elucidation of predictive biomarkers for maternal-child health; (iii) design of affordable, high quality practical biotechnologies; (iv) operationalize systems application through novel modes of healthcare access; and (v) prevention of newborn brain damage; specifically, of bilirubin-neurotoxicities and broncho-pulmonary dysplasia. In addition, he is an avid advocate for maternal, neonatal and child well-being. He is the Co-Founder and Executive Director for the Consortium for Universal Rhesus disease Elimination (CURhE), Co-Founder of NeoDesign (Neonatology), Chair of the Medical/Research Advisory Board of g6pd Deficiency Foundation, Co-Chair of the Audrey K. Brown Kernicterus Symposium at the Pediatric Academic Societies. His awards include the Fellow of the National Neonatology Forum of India and its Lifetime Achievement Award (2014), the Lifetime Achievement Award of Indian Academy of Pediatrics (Neonatology, 2019), the Neonatal Landmark Award by the American Academy of Pediatrics (Section on Neonatal-Perinatal Medicine, 2013) and the “Legend in Neonatology” by MidAtlantic Neonatology, NeoForum (2010). He has pioneered universal pre-discharge neonatal bilirubin screening, global maternal Rhesus blood type screening, point-of-care G6PD testing, neonatal hemolysis screening, assays for bilirubin binding and effective prescription of phototherapy. In addition, he has collaborated in the development novel neonatal thermal support (Embrace device), computerized neonatal function testing (pulmonary graphics) and adaptive oxygen delivery.