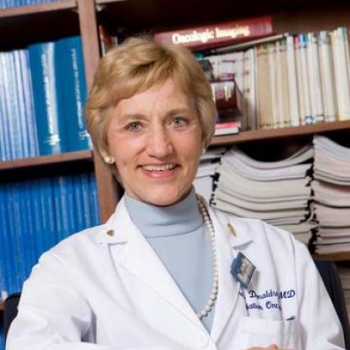
Bio
Sarah S. Donaldson is the Catharine and Howard Avery Professor in the Department of Radiation Oncology at Stanford University School of Medicine. She is also Associate Director of the residency program at Stanford’s Department of Radiation Oncology and Chief of the Radiation Oncology service at the Packard Children’s Hospital in Stanford, California. She is a member of the National Academy of Medicine/Institute of Medicine and a fellow of AAAS, ASTRO, ACR, and ASCO.
Dr. Donaldson has broad expertise in Radiation Oncology with particular interest in Pediatrics, Breast, CNS, Sarcoma Lymphoma, and rare tumors.
She is widely regarded as an authority in pediatric radiation oncology having served as a founding member as the Children’s Oncology Group and the Childhood Cancer Survivor’s Study. She has served as principal investigator on Pediatric Hodgkins Lymphoma, Rhabdomyosarcoma, and Ewings Sarcoma clinical trials.