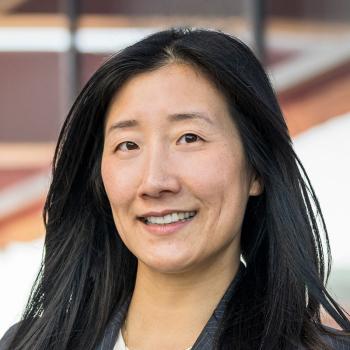
Bio
Dr. Lui studied physics as an undergraduate at Harvard before attending medical school at Johns Hopkins. She completed a general surgery residency at the University of California San Francisco, which included two years of research in the UCSF Thoracic Oncology Laboratory and completion of a Master in Advanced Studies in clinical research. Dr. Lui went on to hold a fellowship in Thoracic Surgery at Massachusetts General Hospital, during which she participated in visiting rotations at Memorial Sloan Kettering and the Mayo Clinic.
Dr. Lui’s surgical practice consists of general thoracic surgery with a focus on thoracic oncology and robotic thoracic surgery. Her research interests include intraoperative molecular imaging for lung cancer localization, increasing rates of lung cancer screening, and using artificial intelligence to predict lung cancer recurrence. She is the recipient of the Donald B. Doty Educational Award in 2019 from the Western Thoracic Surgical Association, the Dwight C. McGoon Award for teaching from the Thoracic Surgery Residents Association in 2020, and the Carolyn E. Reed Traveling Fellowship from the Thoracic Surgery Foundation and Women in Thoracic Surgery in 2022.