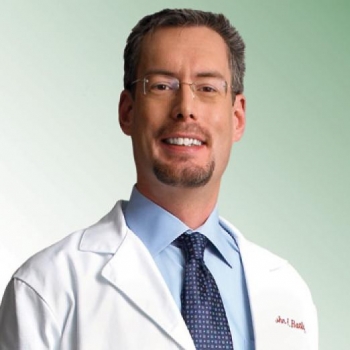
Bio
Dr. John Ratliff is Professor and Vice Chair of Neurosurgery, Departmental Quality Officer, and Co-Director of the Spine and Peripheral Nerve Surgery Division. As a spine surgeon, he treats a diverse array of degenerative spinal conditions. He has a specific research emphasis on quality improvement, decreasing complications in spine surgery, and improving surgical treatment of intramedullary spinal cord tumors.
Dr. Ratliff is Chair of the Joint AANS/CNS Washington Committee. He has served on the Executive Committee of the Congress of Neurological Surgeons and the Joint Section of Disorders of Spine and Peripheral Nerves, is Recording Secretary for the Council of State Neurosurgical Societies, and is on the Board of Directors of Neuropoint Alliance. He is immediate past-chairman of the joint AANS/CNS Neurosurgery Quality Council.