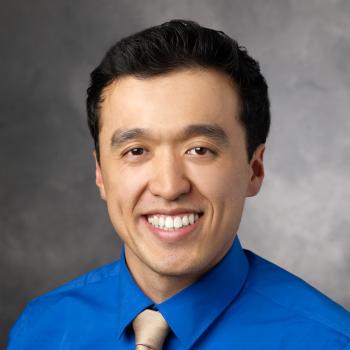
Bio
Ian Chua, MD, MHPE is a bicoastal pediatric hospitalist and assistant professor of pediatrics at Stanford Children’s Health (Palo Alto, CA) and Children’s National Medical Center (Washington, DC). He completed his residency at Stanford Children’s with concentrations in medical education and quality improvement. He obtained his Masters’ in Health Professions Education at University of Illinois in Chicago. He currently directs the ACGME Fellows’ Common Core Curriculum, the PHM Fellowship Medical Education Pathway, and the Pediatric residency medical education pathway at Children’s National Medical Center. His interests have been in educational scholarship and professional development of transitional learners including junior faculty.