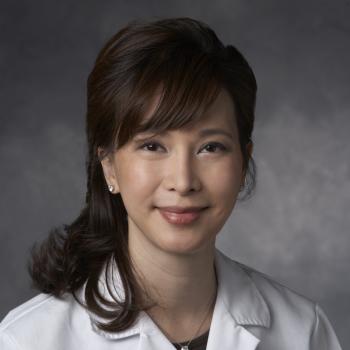
Bio
Dr. Dung H Nguyen is currently the Director of Breast Reconstruction at the Stanford Women’s Cancer Center and the Director of Adult Plastics Clinic at Stanford Healthcare. She graduated with a Bachelor of Science in Biochemistry and highest academic honor and distinction from U.C. Davis. She earned a Pharm.D degree from U.C.S.F. School of Pharmacy and a MD degree from U.C.S.D. She then did a residency in general surgery and a residency in Plastic and Reconstructive Surgery at the University of Southern California (USC) Medical Center. She further completed a fellowship in microsurgery from Chang Gung Memorial Hospital in Taiwan, one of the largest reconstructive surgery centers in the world. She was recruited to Stanford from Cedar Sinai Medical Center in 2012, and is currently a Clinical Professor in the Division of Plastic and Reconstructive Surgery at Stanford University.
Dr. Nguyen specializes in aesthetic and reconstructive breast surgery, surgical treatment of lymphedema including vascularized lymph node transfer and lymphaticovenous anastomosis, and complex tissue reconstruction utilizing microsurgery and supermicrosurgery. She also has interest in cosmetic surgery, including facial rejuvenation and body contouring procedures.
In addition to her clinical commitment, Dr. Nguyen has basic science and clinical research interests in lymphedema and breast reconstruction. She has published articles in peer review journals, presented at national and international professional meetings and has authored book chapters in various plastic surgery textbooks. She also enjoys volunteering on overseas medical missions and participating in medical charity activities.