Bio
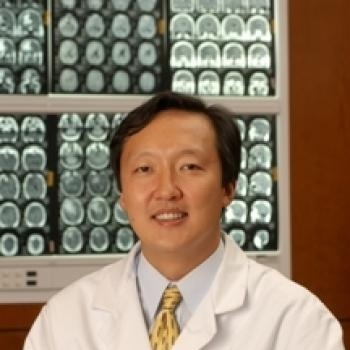
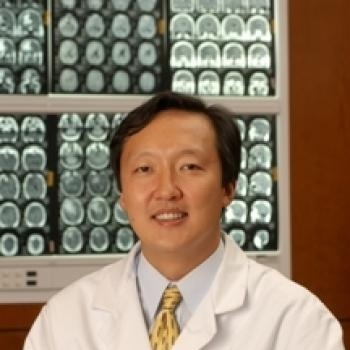
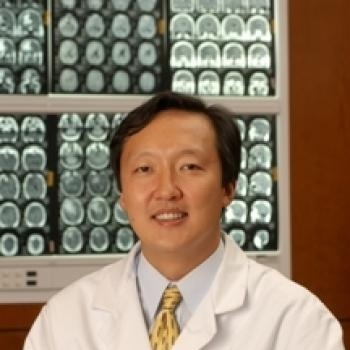
Jon Park, M.D., F.R.C.S.C is the Saunders Family Endowed Professor in Neurosurgery, the Chief of Spine Neurosurgery, Director of Spine Research Laboratory, and Director of Spine Fellowship Program at Stanford University Medical Center. His clinical practice specializes in surgically and non-surgically managing the spinal disorders that affect people's lives, such as debilitating pain and weakness that comes from spine disc problems, spine tumors, spine scoliosis, and spine trauma.
Dr. Park is an internationally recognized leader in the field of spine surgery. He is an active member of American Association of Neurosurgery, North American Spine Surgery, Scoliosis Research Society, and Cervical Spine Research Society. His research focuses on spinal disc regeneration in an effort to target the underlying causes using stem cells and mesenchymal stem cells for inter-vertebral disc regeneration. His research also pioneers in spinal bio-mechanics to apply mechanical principles to ensure spinal stability.