Bio
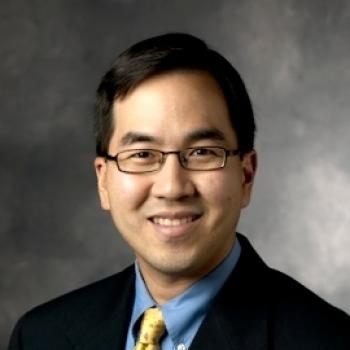
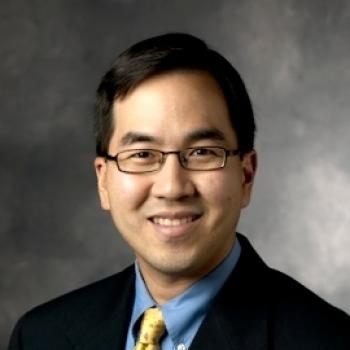
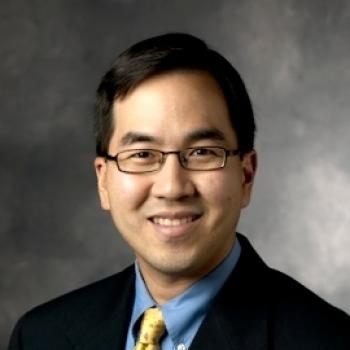
Benjamin I. Chung, MD is a Urologic Oncologist specializing in the treatment of prostate and kidney cancer. As Director of Robotic Surgery, he has one of the largest surgical experiences in robotic prostatectomy and robotic kidney surgeries in the entire state of California and his excellent outcomes have resulted in his election to Castle Connolly Top Doctors and Best Doctors in San Francisco.
Dr. Chung's research focuses upon improving outcomes of surgical management of urologic cancers and in better understanding the causative factors in the formation of these malignancies to allow for future preventative action. Currently, Dr. Chung has an active laboratory focused on the epidemiology of urologic cancer, specifically kidney cancer, to broaden the understanding of what causes kidney cancer. At present, our understanding of the causes and risk factors for kidney cancer remains frustratingly incomplete. There are known risk factors, but scores of unknown correlations that range from toxicologic (chemicals) to pharmacologic (medications) to lifestyle factors that are ripe for discovery.