May 23, 2011 - By John Sanford
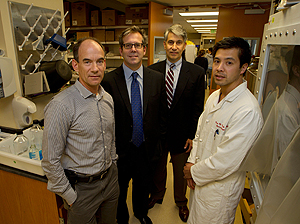
Reinhold Dauskardt, Geoffrey Gurtner, Michael Longaker and Victor Wong collaborated on a new surgical dressing that reduces scar tissue caused by incisions.
Researchers at Stanford University have developed a special wound dressing that they report was able to significantly reduce scar tissue caused by incisions.
Results of animal tests and of an early clinical trial of the dressing were “stunning,” said Michael Longaker, MD, MBA, the Deane P. and Louise Mitchell Professor at the School of Medicine and senior author of a study that details the findings. “It was a surprisingly effective treatment.”
The study was published online May 23 in the Annals of Surgery.
After sutures are removed, the edges of a healing incision are pulled in different directions by the taut, surrounding skin, causing scar tissue to thicken and spread. The novel dressing, which the authors refer to as a “stress-shielding device,” eliminates this tension and hence a considerable amount of scarring.
“This work actually started 20 years ago when I was an intern at Massachusetts General Hospital,” said lead author Geoffrey Gurtner, MD, professor and associate chair of surgery. “I realized early on that we were not going to solve the problem of scarring with current surgical tools and techniques.”
Co-author Reinhold Dauskardt, PhD, professor of materials science and engineering in the School of Engineering, recalled a meeting he had with Gurtner that launched the effort to create a stress-shielding device. “We were talking about our respective research,” Dauskardt said. “Geoff had a lot of experience in wound healing and was thinking about factors that led to scarring. He said, ‘If only we could keep in check the mechanical forces acting on the wound.’ I had multiple programs on skin biomechanics and transdermal-drug delivery. I said, ‘I think I can do that.’”
Dauskardt and his colleagues created the dressing in his lab. It is made of a thin and elastic silicone plastic that is stretched over the incision after sutures have been removed. The dressing sticks to the skin with the help of an adhesive. As it contracts, it provides uniform compression across the wound.
Scar tissue, which is less flexible than regular skin, can cause functional problems, such as limiting motion. Hair does not grow in a scar, and it doesn’t have sweat glands. In addition, scars do not look like regular skin: They are often raised and have a pinkish hue. Many people consider them unattractive. Yet they are an unavoidable side effect of surgery. Every year in the United States, more than 50 million incisions are created during operations. Meanwhile, hundreds of millions of people already have scars that they would prefer to eliminate. Current scar-removal techniques, including surgical excision, steroid injections and laser therapy, are generally expensive, painful or simply not very effective, the authors say.
The researchers predicted the dressing will be used not only to reduce scarring from incisions, but also to make the surgical revision of existing scars a more appealing option; the second scar would be much less visible, if visible at all.
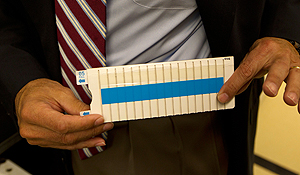
This novel dressing, which Stanford researchers call a “stress-shielding device,” helps to eliminates tension that occurs after sutures are removed when the edges of a healing incision are pulled in different directions by the taut, surrounding skin, which causes scar tissue to thicken and spread.
In pigs, which have skin similar to that of humans, the area of scars caused by roughly 1-inch incisions was reduced six-fold by the stress-shielding device, compared to pigs in a control group with the same-sized incisions, the study said. The stress-shielded wounds “demonstrated nearly scarless closure” eight weeks after sutures had been removed.
The researchers also tested the device on roughly 1-by-1.5-inch excisions — a wound mimicking the kind caused by scar removal — and found that “stress shielding dramatically decreased scar area” compared to unshielded wounds of the same size. “The device seemed to promote regenerative-like repair rather than scar formation,” the authors wrote.
Next, the researchers tested the device on nine female patients who had undergone abdominoplasties (tummy tucks). Given the quantity of tissue removed during this elective surgery, a tremendous amount of tension occurred across the wound after closure. (Scars from these procedures are typically wide and thick.) Longaker said he and his colleagues deliberately chose to test the dressing on incisions closed with high tension: If the dressing could reduce scarring in such cases, it would surely work on any other kind of incision.
One side of the abdomen-wide incision on each patient was treated with the stress-shielding dressing; the other half was not. A panel of three plastic surgeons unaffiliated with the research, as well as a panel of three people not in the medical profession, acted as judges. On a 100-point scale, the lay panel scored the appearance of stress-shielded wounds an average of 13.2 points higher than the control wounds. The expert panel scored the scar appearance of the treated incisions 39.2 points higher. In both of these analyses, the difference between the treated side and the control side were highly significant, the researchers said.
But they noted that some of the wounds demonstrated more dramatic improvement than others. They speculate this may have been due to differences in the amount of tension present in the dressings when they were applied to the wounds. In any case, the researchers cautioned that this was a preliminary clinical study designed only to show “proof of principle in humans.”
“Larger clinical trials are being planned to include greater ethnic diversity within the patient population and to determine the optimal range of stress-shielding forces for anatomic region- and dimension-specific wounds,” the authors wrote.
Other co-authors of the paper, all at Stanford, were: Victor Wong, MD, and Kirit Bhatt, MD, postdoctoral research fellows in the Department of Surgery; Kenneth Wu, PhD, a recent postdoctoral scholar in the Department of Materials Science and Engineering; Ivan Vial, a medical student; Karine Padois, PhD, a postdoctoral scholar in the Department of Materials Science and Engineering; and Joshua Korman, MD, an adjunct clinical assistant professor of plastic and reconstructive surgery.
The research was supported by a Wallace H. Coulter Translational Partners Grant; the Armed Forces Institute of Regenerative Medicine; the Hagey Family Endowed Fund in Stem Cell Research and Regenerative Medicine; and the Oak Foundation.
Neodyne Biosciences Inc. provided the special surgical dressings for the study. Gurtner, Dauskardt and Longaker are founders and hold equity in the company.
About Stanford Medicine
Stanford Medicine is an integrated academic health system comprising the Stanford School of Medicine and adult and pediatric health care delivery systems. Together, they harness the full potential of biomedicine through collaborative research, education and clinical care for patients. For more information, please visit med.stanford.edu.