February 14, 2011 - By John Sanford
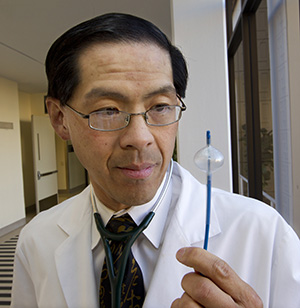
Paul Wang is one of the inventors of a treatment for an abnormal heart rhythm, paroxysmal atrial fribrialtion. It uses an icey cold balloon catheter to get rid of problematic heart tissue.
Eugene Tsuji was biking on a trail in the Forest of Nisene Marks State Park in Aptos, Calif., when his heart monitor went bananas.
“It took off to about 160 beats per minute and then dropped to 50. It seemed confused. Then it went back to normal,” recalled Tsuji, 47, an avid cyclist, of that day in 2003. “I didn’t notice any symptoms at that point, so I blew it off. I figured there was something wrong with it.”
Over the next four years, he tried other heart monitors, but each would occasionally display the same kind of erratic numbers. As it turned out, the problem wasn’t with the monitors; it was with Tsuji’s heart: He had paroxysmal atrial fibrillation, an abnormal heart rhythm that would come and go for periods ranging from a few seconds to a few hours. “It would feel like a slight hiccup in my chest,” he said.
Tsuji was referred to Paul Wang, MD, an expert on atrial fibrillation at Stanford Hospital & Clinics. As part of a clinical trial, Wang and his associates were employing a novel balloon ablation catheter, Medtronic Inc.’s Arctic Front, to treat the disease. The device destroys the problem-causing heart tissue by freezing it. Tsuji signed up for the trial. Now, after more than three years with virtually no symptoms, he’s glad he did.
In December, the new device earned approval from the U.S. Food and Drug Administration. Stanford Hospital is one of the few California hospitals now offering it for the treatment of paroxysmal atrial fibrillation that does not respond to drug therapy. It is the first catheter in the United States specifically designed and approved for treating this disease. Its freezing technology was invented by Wang and two other medical scientists in the late 1980s. Wang is now a consultant for Medtronic.
Atrial fibrillation affects some 2.2 million Americans. Risk factors include old age, high blood pressure, sleep apnea and heart disease. The problem stems from chaotic electrical impulses in the upper chambers — the atria — of the heart. A normal heart contraction begins with an electrical signal from the sinoatrial node, a group of cells in the right atrium. In atrial fibrillation, however, signals are sent from other parts of the atria, disrupting the regular cardiac rhythm. These abnormal signals tend to originate where the pulmonary veins empty into the left atrium.
If you observe the heart when the disease is acting up, it looks like a quivering bowl of Jell-O. Symptoms can be subtle and painless, as they were in Tsuji’s case, or include shortness of breath, fatigue, lightheadedness and chest pain. In any case, the condition can lead to serious complications: The chaotic rhythm may cause blood to pool in the atria, forming clots. If a clot dislodges, it may travel to the brain and block a blood vessel, causing a stroke. Untreated paroxysmal atrial fibrillation can become chronic, resulting in persistent heartbeat irregularities.
“A-fib tends to aggravate itself, meaning the longer you remain in it, the harder it is to get rid of it,” said Wang, who is also a professor of caridovascular medicine.

Eugene Tsuji, an avid cyclist, was surprised that he had an abnormal heart rhythm. A novel treatment at Stanford Hospital fixed the issue.
There are several common ways to treat the disease: For patients with the persistent form, in which the rhythm does not go back to normal by itself, doctors can administer an electrical shock to the heart (cardioversion), which resets the rhythm. Medication can also be prescribed to help maintain a normal heartbeat, but many patients do not respond to drug therapy. This was Tsuji’s experience and why he was allowed to participate in the clinical trial. Another option is radiofrequency catheter ablation, which heats and kills the tissue responsible for sending out the erratic impulses.
“Ablating these specific areas allows blood to flow but stops the electrical signals that are responsible for the heart rhythm problem,” Wang said.
However, currently available radiofrequency catheters were designed for other heart rhythm problems, not for atrial fibrillation. They have a small tip, which makes the process slow and painstaking. But the catheter with which Tsuji was treated, the Arctic Front, features a super-cold balloon that expands to contact all sides of the atrial wall outside the pulmonary-vein openings, like a beach ball wedged in the top of a barrel. It ablates a larger swath of tissue at one time.
Tsuji came in for the cryoablation treatment in 2007. He stayed one night at the hospital and then returned home. “I needed to rest for a couple of days but didn’t feel bad,” he said.
Results of the clinical trial in which he participated showed that about 70 percent of patients who underwent cryoablation remained free of the heart problem after one year, compared with about 7 percent of those given drug therapy. (The trial was sponsored by CryoCath Technologies Inc., which Medtronic has since acquired.)
Today, Tsuji is almost completely free of the condition and symptoms. “The only time I’ve ever really noticed the feeling of the heart hiccup again is when I’m really hot and I drink something really, really cold,” he said. “But I would basically say it’s nonexistent now. My heart does what it’s supposed to do.”
John Sanford is a writer in Stanford Hospital’s communications office.
About Stanford Medicine
Stanford Medicine is an integrated academic health system comprising the Stanford School of Medicine and adult and pediatric health care delivery systems. Together, they harness the full potential of biomedicine through collaborative research, education and clinical care for patients. For more information, please visit med.stanford.edu.