June 7, 2010 - By Ruthann Richter
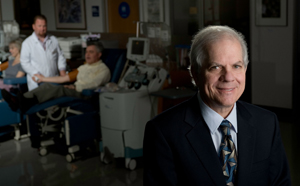
Ed Engleman played a vital role in the effort to develop a cancer vaccine, which the FDA recently approved for treating late-stage prostate cancer.
When the federal Food and Drug Administration approved the first therapeutic cancer vaccine April 29, it was sweet news indeed for Ed Engleman, MD, director of the Stanford Blood Center. That kind of therapy was just what Engleman had in mind more than 18 years ago when he conceived the idea of tricking the immune system into fighting cancer.
“One of the core questions of immunology and cancer has been whether this approach can be effective,” said Engleman, a cellular immunologist and professor of pathology. “To me, it breaks open a huge wall in proving an idea that people seriously questioned. So this is really going to be door-opening.”
The new vaccine, known by the trade name Provenge, has been approved by the FDA for use in men with advanced prostate cancer who have failed all other treatments. It was approved after a long and arduous series of clinical trials by the maker, Seattle-based Dendreon, which showed that men on the vaccine lived an average of four months longer than those on placebo.
Engleman founded Dendreon, together with Samuel Strober, MD, professor of medicine at Stanford, in 1992. Neither of them has been involved in the company for a decade, but to this day, they continue to build on their early work, with the goal of developing an even more potent cell-based treatment that would cure solid tumors.
Dendreon’s newly approved vaccine is built around a rare cell of the immune system, known as the dendritic cell, so called because it has long, fingerlike projections that help it interact with its environment. Engleman began studying these cells when he first joined the faculty at Stanford in 1978. In fact, he said one of the main reasons he agreed to direct the newly formed blood center was because it would give him ready access to these and other white blood cells of the immune system for research purposes.
These white cells are routinely removed when people donate blood, as they might cause harm if given to patients whose immune systems are compromised. So the blood center has a ready source for these cells, which have been the focus of hundreds of valuable research projects over the years. Engleman notes that the blood center, one of the few in the country located in a medical school, was created not only to provide blood products to the hospitals but also to support research and teaching. Without the close relationship between researchers and blood center staff, as well as the generosity of donors, the group’s dendritic cell work would not have been possible, he said.
In the early days of the blood center, Engleman became interested in the dendritic cell because it has the powerful ability to recognize foreign proteins and then alert T cells, the foot soldiers of the immune system, to respond. But little else was known about the cells at the time; they had been isolated in mice, but not yet in people.
“We thought that if we could find and isolate them in humans, we could better understand their functions and think about how they might be useful,” Engleman said. Two postdoctoral fellows in his lab were able to accomplish that in 1989, publishing their work in the Journal of Clinical Investigation in 1990.
Then Engleman began to consider the possibilities: What if scientists could isolate dendritic cells in cancer patients and somehow train the cells to attack the cancer? It was a difficult immunologic question because the immune system typically doesn’t attack cells that it views as “self,” and tumor cells are seen as self. “So most immunologists would have said this is an impossible undertaking,” Engleman said.
His concept was to take the dendritic cells out of their native environment, away from the tumor, by removing them from the patient. Then they could be exposed in the lab to a specific cancer-related protein that would prime them for action. These newly trained cells then could be infused back into the patient, where they would target the cancer.
With that idea in mind, he teamed up with Strober in 1992 to launch Activated Cell Therapy Inc., which would later be renamed Dendreon. While Engleman was interested in enhancing the immune response, Strober was primarily interested in ways of suppressing the immune response in conditions such as autoimmune disease or organ rejection. Strober also had developed a commercially viable method for rapidly enriching and purifying immune cells for various uses. Dendreon licensed the technology from Stanford, and still has patents pending.
Engleman began testing out his idea on a dendritic cell therapy with Ronald Levy, MD, professor and chief of the division of oncology, who also was working on approaches to vaccinate cancer patients against their own tumors. In 1996, they published a paper in Nature Medicine involving four patients with B-cell lymphoma who were infused with a vaccine made of stimulated dendritic cells. All of the patients had measurable responses, with tumors that receded or, in one case, disappeared altogether. They went on to do trials in a larger number of patients, reporting in 2002 in the journal Blood on 35 patients with B-cell lymphoma who were treated with a similar vaccine. Results again looked promising. Engleman and colleagues continued to do work with the dendritic cell vaccines in other cancers, including prostate, colon and lung cancer. In 2001, he and Stanford colleagues reported results of an early-phase trial using immunotherapy in 12 patients with metastatic colon or lung cancer. Two of the 12 patients showed dramatic tumor regression, one patient had a mixed response, and two saw their disease stabilized. In the remaining patients, the tumor continued to progress.
In 2000, Dendreon moved to Seattle, and both Engleman and Strober discontinued their relationship with the company. Engleman still owns shares of company stock.
Dendreon went on to use the dendritic cell approach with a focus on metastatic prostate cancer, conducting clinical trials in more than 700 men with advanced disease. In the final trial, which was conducted in 512 patients, of those who received the dendritic cell treatment, 31.7 percent were alive at three years, compared to 23 percent of those who received placebo. The treatment was deemed safe, as the primary side effects – chills, fatigue, fever, back pain, nausea, joint ache and headache – were mild. The average life extension for men on the treatment was four months.
The FDA approval of the vaccine was considered a milestone, with oncologist Leonard Lichtenfeld, MD, deputy chief medical officer for the American Cancer Society noting in his blog that “it reinforces for many the dream that one day we would be able to turn on the body’s own defense mechanisms as one more approach to treat (or one day perhaps prevent) certain cancers.” Still, he noted the limitations of the vaccine, which could not be considered a “miracle cure.”
Strober agreed.“Dendreon really is just the beginning of the road,” he said. “It’s an important milestone, but it didn’t cure prostate cancer, so there’s a lot of work yet to be done.” He and Engleman are now working on another approach to treatment of solid tumors that combines a more potent dendritic cell therapy combined with hematopoietic cell transplantation. Hematopoietic cell transplantation (also known as bone marrow transplantation) is commonly used in leukemia and lymphoma, but not for solid tumors. The two scientists have developed a mouse model using this double-punch therapy for metastatic colon cancer. “We’re able to cure large primary tumors in the mouse model,” Strober said. “So our hope is to go from that mouse model to clinical trials in the next year or two and see what works. It’s an important extension for the kind of work that Dendreon is doing.”
About Stanford Medicine
Stanford Medicine is an integrated academic health system comprising the Stanford School of Medicine and adult and pediatric health care delivery systems. Together, they harness the full potential of biomedicine through collaborative research, education and clinical care for patients. For more information, please visit med.stanford.edu.